Healthcare is better than ever in many ways. Thanks to improvements in research and technology, providers and systems can screen and treat people early and better, which helps many people avoid health problems that could disrupt their lives or cause early death. But the ability to provide this kind of care is not the same as actually providing it. Too often, minority groups are left out of innovation and don’t receive equal access to care.
In the US, many people who identify as part of minority groups have experienced unfair treatment in healthcare settings.
Many factors contribute to these healthcare disparities, one of which is bias. This article discusses implicit bias, how it manifests, how it differs from explicit bias, and what you can do to prevent it from affecting your patients.
Implicit Bias and Health Disparities
Implicit or unconscious bias is a belief someone holds about other people without being aware. These unconscious beliefs affect our behaviors and opinions and drive assumptions based on stereotypes.
Implicit bias can create places where people who identify with a minority don’t feel comfortable expressing themselves, even if there is nothing overtly discriminatory in the space. It also affects how we treat others; for example, some people may cross the street if they see someone coming toward them with certain characteristics they’ve been taught to assume as unsafe.
Unconscious bias is especially serious in settings where someone’s decision impacts the other person, like a medical emergency.
For example, people of color receive less pain medication than white patients under the same circumstances. Statistically, women of color are more likely to experience complications and death during childbirth. And they’re more likely to receive a delayed diagnosis of heart disease, affecting their recovery and survival. This gap in care is down to bias blind spots, whether intentional or implicit/unconscious, which leave out vast swaths of the population.
These health disparities also mean that chronic illnesses and other health concerns disproportionately burden many populations. More African Americans and Latinos, compared to whites, have at least one of seven chronic conditions: asthma, cancer, heart disease, diabetes, high blood pressure, obesity, or anxiety/ depression.
This is partly because they don’t get treated quickly or at all, compared to white populations.
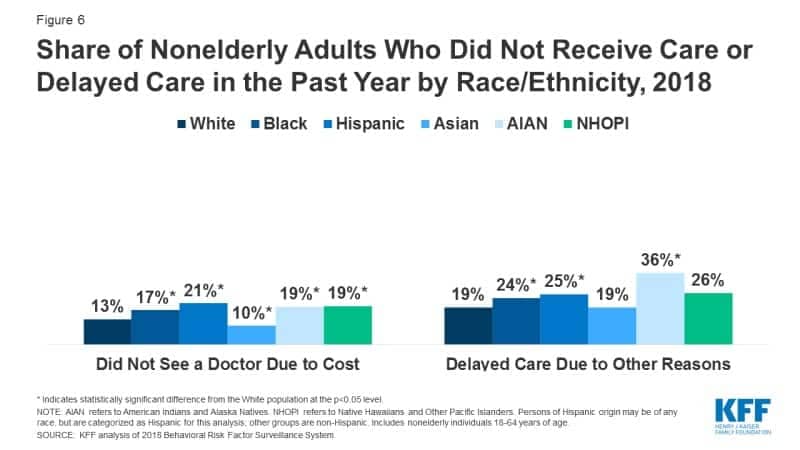
Source: KFF
Healthcare leaders can’t ignore these figures. So it’s imperative for agencies to understand health disparities and develop cultural competence among their team.
Hybrid learning is here to stay. This e-course covers everything you need to know about how to prepare for a hybrid learning project, from earning buy-in to the must-have elements for successful virtual collaboration. Access it here.
Conscious vs. Unconscious Bias
Implicit bias is something people are unaware of. So they act unconsciously and usually mean no harm. However, this doesn’t mean that their actions are harmless, as actions resulting from implicit bias often have deep, long-term effects on those experiencing the consequences. In fact, one characteristic of implicit bias is that, usually, the only people aware of it are those damaged by it.
Conversely, when exercising explicit, or conscious, bias, the individual intends to distance themself from the person they perceive as different. So they’re well aware of their biases and do nothing to mitigate them. Explicit bias can lead to dangerous situations for those discriminated against in the form of violence, or in the medical context, a lack of resources and attention.
Implicit bias can become explicit when the person becomes aware of their prejudice and continues to hold it instead of working to address it.
What Is Cultural Competence?
The American Psychological Association defines cultural competence as “the ability to understand, appreciate and interact with people from cultures or belief systems different from one’s own.“
In short, cultural competency means being able to help the people in your community have better access to appropriate healthcare and their best possible health. It also means working within the context of your clients’ cultural beliefs, behaviors, and needs. So cultural competency is an essential element that bridges the people in your community and the healthcare system.
In terms of services and care, this might look like some of the following:
- Providing interpreters when necessary
- Addressing gaps in health literacy
- Recruiting and training a culturally diverse team
- Setting up clinics and providers to offer transgender care
- Providing training to all staff in cultural awareness, knowledge, and skills
- Collaborating with traditional healers
- Offering specialized training on LGBTQ+ health issues
- Hiring and training community health workers
- And finally, recognizing and applying culture-specific attitudes in health promotion
Note that these practices are both inward-facing and outward-facing for healthcare agencies. Yes, it’s about having a diverse team, but it’s also about knowing how to talk to a diverse community. So you must be fully aware of your organization for that to extend to your client community.
Providing Cultural Competence Training
To create a workplace with cultural competence, you’ll need to invest in change, including continued learning, listening, and evolving because health professionals need to learn how to deliver services with awareness and sensitivity.
The first step is to invest in ongoing training covering various topics. To start, look for or create training programs that cover areas such as:
Health disparities and social determinants of health. Develop a thorough understanding of the impact of socioeconomic and sociocultural factors on clients, patients, and providers.
Implicit bias training for healthcare providers. While explicit bias is obvious, implicit bias is not. For example, overt racism and prejudice are clear. It’s harmful but easier to spot. Unconscious bias is more insidious and pervasive because people don’t recognize it. So implicit bias training can address harmful stereotypes. In fact, implicit bias training is mandatory in many states.
Health literacy. Improving the understanding of health information in a context that makes sense for the patient and client.
Eliminating language barriers. In essence, working with medical interpreters, providing language proficiency courses, or working with bilingual staff.
Communication skills. Developing language skills to include wider ways of communication in the healthcare system, including patient, provider, insurance, and administration, so patients navigate the system more effectively.
However, it’s worth noting that one short course is just the beginning and not a one-and-done thing. Instead, cultural competence in healthcare is a process and a way of operating. It pays off to expand your institution’s capacity in cultural competency and diversity because it improves health outcomes, builds community relations, and supports a stronger internal culture.